Chapter 10 IVC Measurement
10.1 Measurement Location
Even a beginning echocardiographer usually finds the inferior vena cava (IVC) quite easily from the subcostal projection. However, in some patients, the subcostal window doesn’t offer any diagnostic visibility, which may be due to, for example, bowel gas.
I have noticed that beginners sometimes confuse measurements between the inferior vena cava and abdominal aorta. To solve this, I have launched a principle by which they can be easily distinguished from each other (Figure 10.1):
- first the inferior vena cava is identified by tilting, which I call “liver tilt”
- after this, the abdominal aorta is identified by “spleen tilt”.
Once both the inferior vena cava and abdominal aorta have been identified, they cannot be confused with each other.
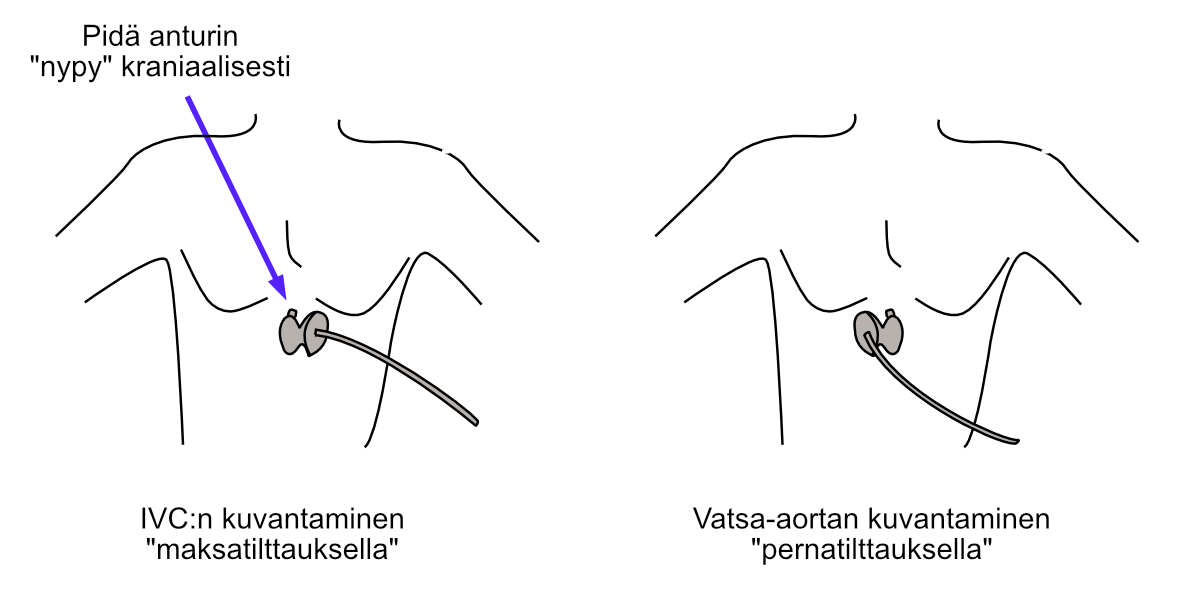
Figure 10.1: Identification of inferior vena cava and abdominal aorta using “liver and spleen tilting”.
10.2 2D Image Measurement
I recommend measuring the inferior vena cava (IVC) from 2D images. Often you cannot get a completely perpendicular cut of the IVC from M-mode, and achieving such a cut takes unnecessary time, especially from a beginner.
The IVC should not be measured right at the hepatic vein junction but about 1-3 cm “toward the feet,” as demonstrated in the image below (Figure 10.2).
Images are recorded from the IVC both during expiration and inspiration. You don’t need to think separately about which phase of breathing was going on: simply measure the IVC at the same location at its widest and narrowest.
I recommend that you try to get some view of the right atrium as well (Figure 10.2). The IVC connects to the right atrium, so you can be sure you’re taking measurements from exactly the IVC. Transducer tilts, which I already presented above, also help in IVC identification (Figure 10.1).
Note! The limitations of IVC measurements in fluid status assessment must be recognized!
I recommend reading, for example, Marik and colleagues’ review on the topic. For example, significant tricuspid regurgitation can complicate volume status assessment based on the IVC, of which I also have plenty of clinical experience.
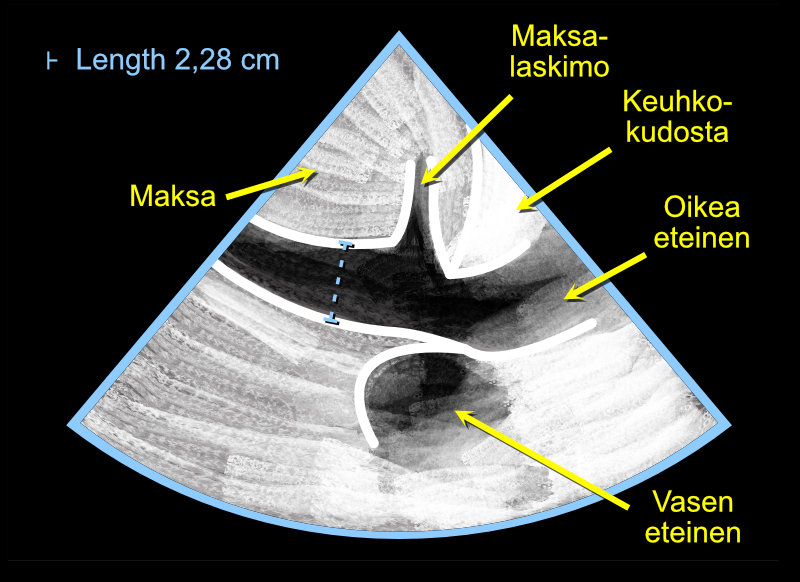
Figure 10.2: Measuring the diameter of the inferior vena cava (IVC) using the Caliper button. Note. Measure the diameter both during expiration and inspiration.
10.3 CVP Inference from IVC
Echocardiography umbrella organizations have presented a very simple principle by which CVP can be inferred from the IVC in an instant. This principle is presented in the following table.
| Condition | CVP (mmHg) | Interpretation |
|---|---|---|
| IVC ≤ 2.1 cm and collapses > 50 % with ‘sniffing’ | 3 | CVP normal |
| IVC > 2.1 cm and collapses < 50 % with ‘sniffing’ | 15 | CVP high |
| all other possible measurement scenarios | 8 | CVP moderate |
Examples:
| Finding | CVP (mmHg) |
|---|---|
| IVC 1.5 cm and collapses > 50 % | 3 |
| IVC 2.7 cm and collapses < 50 % | 15 |
| IVC 1.5 cm but collapses < 50 % | 8 |
| IVC 2.7 but collapses > 50 % | 8 |
Echo Guidebook © 2022 by Ville Langén is licensed under CC BY-SA 4.0